Table of Contents
ToggleThe follicle-stimulating hormone, commonly known as FSH, plays a key role in the reproductive system of both men and women. It is essential in regulating the menstrual cycle, the production of eggs and sperm, and overall fertility. Understanding the impact of FSH can offer deeper insights into reproductive health and potential difficulties in conceiving.
Although FSH tests are still performed during the early days of the cycle, values may vary across cycles in the same woman. That is why ovarian reserve is usually assessed with ultrasound and anti-Müllerian hormone (AMH) levels, which can be measured at any point in the cycle.
In this article, we explore what FSH is, how it functions in the body, its normal ranges, and how it impacts fertility in both men and women. We also cover related hormonal studies used to evaluate fertility.
What is the FSH hormone?
FSH is a gonadotropin hormone produced by the pituitary gland at the base of the brain. Together with luteinizing hormone (LH), FSH is essential in regulating the menstrual cycle and reproductive function. Its main role is to stimulate the growth and maturation of ovarian follicles in women and sperm production in men.
To evaluate reproductive health, FSH levels are typically measured via blood tests during the first days of the menstrual cycle. Normal FSH levels vary depending on the phase of the cycle, age, and overall health.
FSH in women
In women, FSH is crucial for the development of ovarian follicles. During each menstrual cycle, FSH levels rise in the follicular phase (the first half of the cycle), encouraging follicle growth. One dominant follicle matures and releases an egg at ovulation, which is necessary for conception.
Normal FSH levels in women
FSH levels fluctuate throughout the menstrual cycle. Here are approximate values for each phase:
- Follicular phase: 2.5 – 10.2 mIU/mL
- Ovulation phase: 3.4 – 33.4 mIU/mL
- Luteal phase: 1.5 – 9.1 mIU/mL
- Menopause: 23 – 116.3 mIU/mL
- Pregnancy: less than 0.3 mIU/mL
FSH levels naturally rise with age as ovarian reserve declines. Higher levels may indicate reduced fertility, as more stimulation is required for the ovaries to function effectively.
FSH and conception
When trying to conceive, it’s ideal to have FSH levels below 10 mIU/mL in the follicular phase. Values above 12 mIU/mL may suggest diminished ovarian reserve, potentially complicating natural conception.
In fertility treatments such as IVF, FSH levels help tailor hormonal medication and determine the best protocol. FSH-based medications are also used to stimulate the ovaries and increase the success rate of egg retrieval.
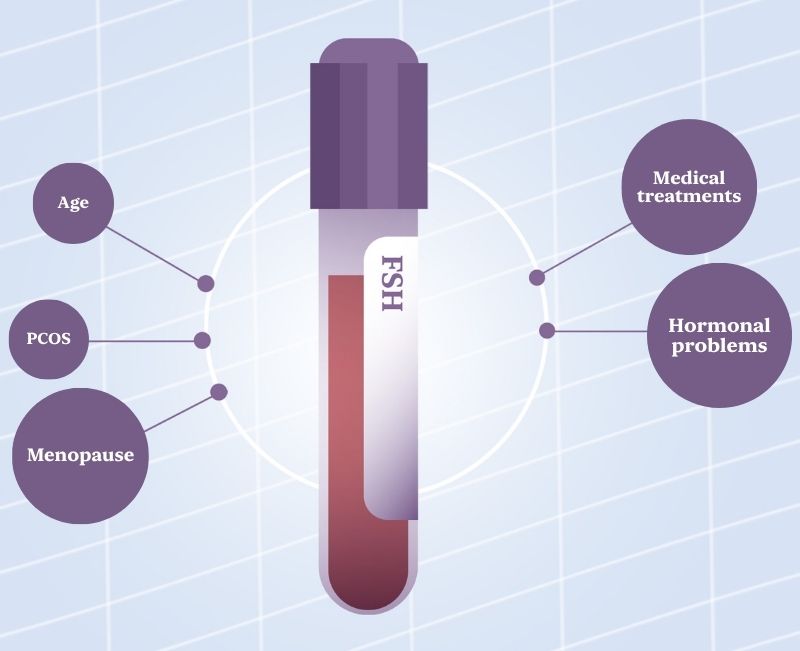
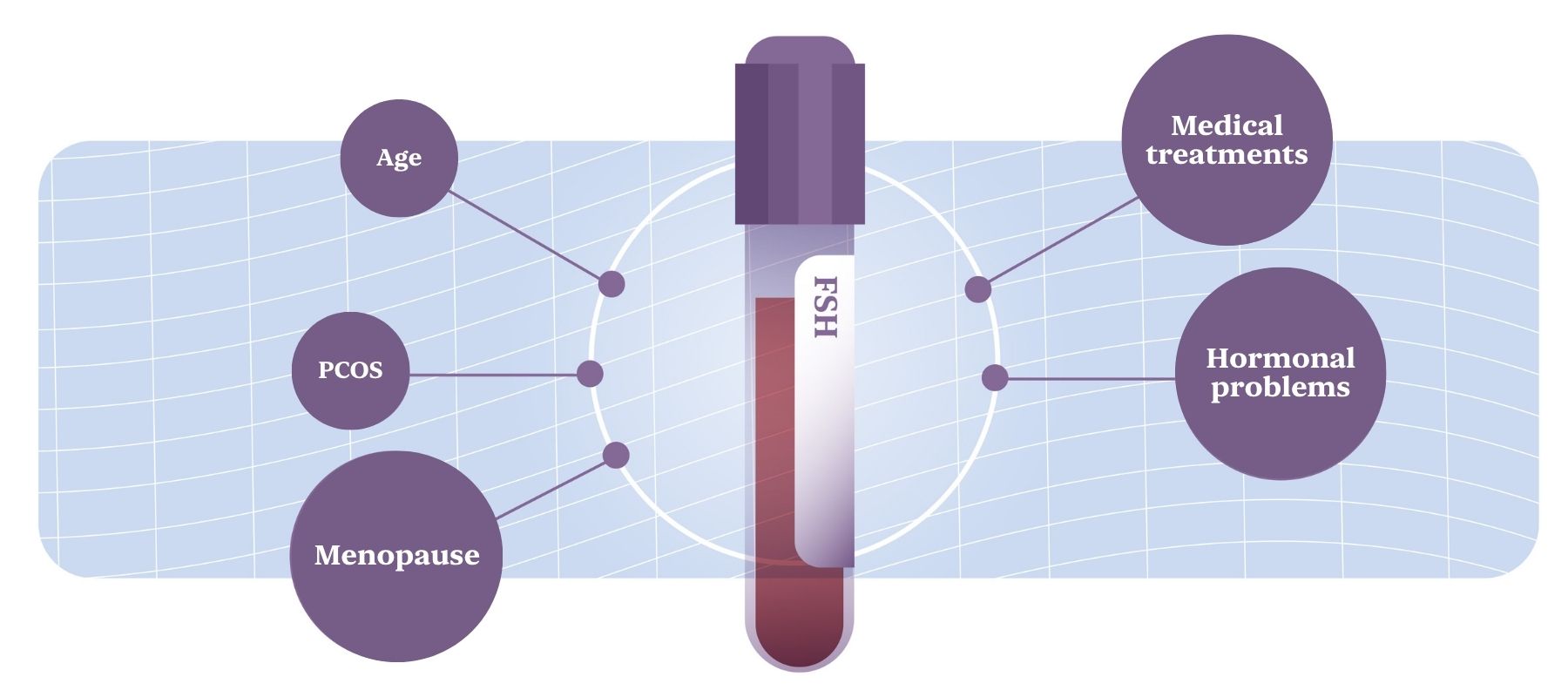
Factors affecting FSH levels
Several factors can influence FSH levels. Some are temporary, while others are long-term. These include:
- Age: Levels naturally rise, especially after age 35.
- Menopause: FSH levels increase significantly as ovarian activity ceases.
- Hormonal disorders: Conditions like PCOS or pituitary dysfunction can alter levels.
- Medical treatments: Hormone therapies and radiation may affect FSH levels.
FSH in men
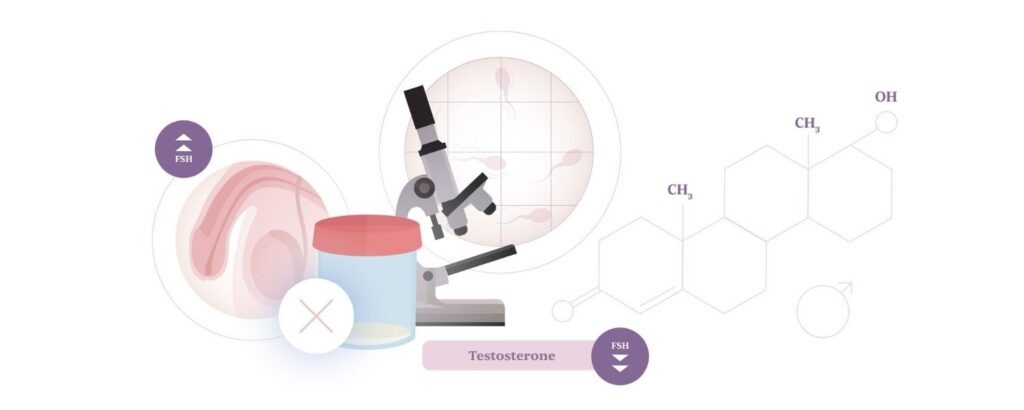
In men, FSH stimulates the testicles to produce sperm within the seminiferous tubules. Although testosterone is also important, FSH is essential for spermatogenesis. Abnormal levels may indicate testicular issues or fertility problems.
Normal FSH levels in men
- Adult men (21+): 1.4 – 18.1 mIU/mL
- High FSH: May indicate primary testicular failure (testicles not responding properly).
- Low FSH: Could signal hypogonadism (insufficient hormonal stimulation).
If a man is facing infertility, FSH testing is commonly paired with other hormone panels and semen analysis.
What if my FSH levels are not normal?
Abnormal FSH results are not necessarily conclusive. Hormone levels fluctuate, and a single test may not provide a full picture. Your doctor may order follow-up tests or combine FSH results with other hormone evaluations to assess reproductive health.
For women, elevated FSH levels may prompt an ultrasound or an anti-Müllerian hormone (AMH) test, which more precisely assesses ovarian reserve. AMH is useful in planning conception or fertility treatments. Learn more about AMH testing here.
Understanding your FSH levels is a key step in making informed decisions about your reproductive health. Consult a fertility specialist to evaluate your unique situation and identify the most appropriate solutions.
If you have concerns, feel free to contact our team.