Table of Contents
ToggleFor many people, the desire to start a family is one of life’s most meaningful goals. However, the journey to parenthood can sometimes include the painful experience of a miscarriage. This event, while emotionally difficult, is more common than people think, and is often wrongly perceived as a personal failure. At Next Fertility, we want to help you understand that having a miscarriage does not make you any less capable of becoming a parent.
More than 15% of pregnancies end in miscarriage during the first weeks, often without a specific cause doctors can identify. Normalising the experience of miscarriage is essential so that people going through it understand they are not alone—and that in many cases, it’s just one step in the reproductive process.
However, when miscarriages become recurrent—two or more consecutive pregnancy losses—it is normal to feel concerned. Should I be worried? Should I seek help? Is there anything I can do?
What is a miscarriage and why does it happen?
A miscarriage is the loss of a pregnancy before the 20th week of gestation. This is more common than many believe—it occurs in about 15–20% of pregnancies, especially during the early weeks. While the emotional pain may be deep, it is important to understand that most miscarriages happen due to factors beyond the pregnant person’s control and are not necessarily a sign of infertility issues.
Why can a miscarriage be considered normal?
The human body has natural mechanisms that may end a pregnancy if the embryo is not developing properly. This can be a biological response to issues that could affect the future health of the baby. Most of these losses occur in the first few weeks and can be caused by random factors such as genetic abnormalities in the embryo that the body detects early on.
Main causes of miscarriage
Most miscarriages are due to natural factors affecting the embryo in the early stages of development. The most common causes include:
Genetic abnormalities
Miscarriages are often caused by chromosomal abnormalities that prevent healthy embryonic development. In these cases, the body naturally stops a pregnancy that would not progress properly.
Hormonal problems
Lack of certain hormones, such as progesterone, can affect the embryo’s ability to properly implant in the uterus and develop in the early stages.
Maternal health conditions
Chronic illnesses like poorly managed diabetes, thyroid issues, or autoimmune disorders can increase the risk of miscarriage.
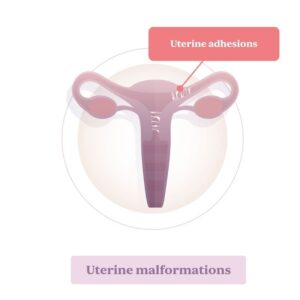
Uterine factors
Uterine malformations or conditions like Asherman’s syndrome (intrauterine adhesions) can interfere with implantation and embryo development.
External factors
Exposure to certain medications, serious infections, or substances like alcohol and tobacco can raise the risk of miscarriage.
Understanding these causes can help people who have experienced a miscarriage find comfort in knowing that, in most cases, it is not the result of something they did or didn’t do.
Recurrent Miscarriage: When Should I Worry?
While having one miscarriage may be considered part of the reproductive experience for many people, having two or more consecutive miscarriages can raise questions about underlying causes. In such cases, it’s advisable to visit a fertility clinic for a complete evaluation to identify possible reasons behind the losses.
What is a recurrent miscarriage?
Recurrent miscarriage refers to the loss of two or more consecutive pregnancies before the 20th week. This condition affects approximately 1% of people of reproductive age and is often linked to medical factors that can, in many cases, be identified and treated to improve chances of future pregnancy success.
Possible causes of recurrent miscarriage
Some of the most common causes that may contribute to recurrent pregnancy loss include:
Genetic factors
Genetic alterations in one or both partners may cause issues in embryo development, resulting in recurrent losses.
Immunological problems
Certain immune system disorders can cause the body to reject the embryo as if it were a foreign substance, preventing its proper development.
Uterine abnormalities
Malformations such as a uterine septum or fibroids can make it harder for the embryo to implant and grow.
Hormonal imbalance
Conditions like polycystic ovary syndrome or low progesterone levels may affect the embryo’s ability to remain implanted.
Medical conditions
Diseases such as lupus, clotting disorders, or hyperthyroidism may increase the risk of miscarriage.
Physical and emotional recovery
Physically, the body usually recovers quickly after a miscarriage, especially if it occurs in the early weeks of pregnancy. However, emotional recovery may take longer, and it’s essential to have support to process the experience. Talking to others who have been through it and seeking both medical and emotional guidance can be very helpful.
If you have had one miscarriage, remember that you are not alone—and in most cases, it does not prevent future pregnancies. If you’ve had more than one, it may be time to look deeper into the situation, which we address in the next section.
Book your first consultation
Request your appointment and get your first diagnosis. We want to hear your story.