A bicornuate uterus refers to a congenital uterine malformation. In these cases, the uterus has a heart-shaped appearance divided into two “horns.” It is a relatively common condition and may affect around 1% of women. But what happens if you have a bicornuate uterus? In this article, we aim to clarify its causes, treatment options, and the possible implications of being born with this condition.
Table of Contents
ToggleCauses of a Bicornuate Uterus
A bicornuate uterus is a condition that develops during embryonic growth, when the Müllerian ducts—which form the uterus—fail to fuse completely. Although the exact causes are still unknown, genetic, hormonal, and environmental factors are believed to play a role.
Genetic Factors
Scientific evidence supports the influence of genes and mutations in the abnormal development of the Müllerian ducts and, therefore, of the uterus. Certain genes have been linked to this type of malformation.
Hormonal Factors
Hormones play an important role in the development and differentiation of the reproductive organs during embryonic life. Any hormonal imbalance during this critical period may result in a bicornuate uterus.
Environmental Factors
According to recent studies, fetal exposure to certain chemicals or toxins may increase the risk of uterine malformations, including a bicornuate uterus. However, ongoing research continues to explore the exact connection between environmental factors and this congenital condition.
Symptoms of a Bicornuate Uterus
In some cases, this condition can go unnoticed because many women do not experience obvious symptoms. Some only discover they have a bicornuate uterus when facing difficulties becoming pregnant or experiencing pregnancy complications.
However, certain symptoms are relatively common among women with this condition.
Pelvic Pain
Some women may experience chronic pelvic pain. This may be due to the abnormal anatomy of the uterus, which puts pressure on surrounding organs and causes persistent discomfort.
Severe Menstrual Cramps
This occurs because menstrual flow may have difficulty exiting or may accumulate within the uterine horns. This can lead to stronger, more painful contractions during menstruation.
Irregular Menstrual Bleeding
Women with a bicornuate uterus may experience irregular cycles, longer or shorter periods, or spotting between menstrual cycles.
Difficulty Achieving Pregnancy
This malformation can affect fertility. The abnormal shape of the uterus may hinder embryo implantation and normal gestational development. However, this does not mean pregnancy is impossible or that all women with this condition will face fertility challenges.
Symptoms can vary greatly, and some women may never experience any discomfort.
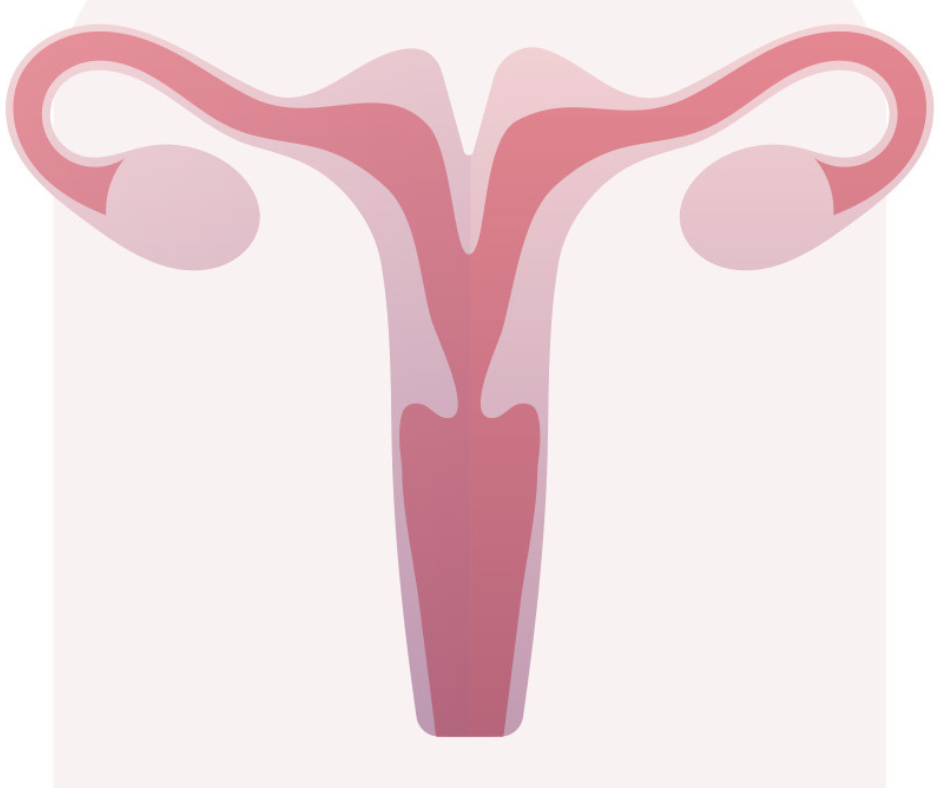
How Is a Bicornuate Uterus Diagnosed?
Women typically discover this condition during a routine gynecological exam or when seeking care for difficulty achieving pregnancy. Diagnosis is usually made through imaging tests that allow the specialist to assess uterine structure.
Transvaginal Ultrasound
This is the most commonly performed imaging test. A probe is inserted into the vagina to obtain detailed images of the uterus. When using 3D or 4D technology, ultrasound becomes the ideal method for diagnosing a bicornuate uterus.
Hysterosalpingography
This radiological procedure involves injecting contrast fluid through the cervix to visualize the uterus and fallopian tubes via X-ray, allowing detection of structural abnormalities.
Magnetic Resonance Imaging (MRI)
MRI provides highly detailed images of internal organs and is particularly useful for assessing uterine anatomy and detecting malformations such as a bicornuate uterus.
These tests help the specialist confirm the diagnosis and evaluate the type and severity of the malformation.
Treatment for a Bicornuate Uterus
A bicornuate uterus does not always require treatment. The best approach depends on symptoms, severity, fertility goals, and the woman’s overall health. A specialist will determine the most appropriate plan.
Conservative Management
If the bicornuate uterus causes no symptoms, treatment may not be necessary. However, periodic monitoring is usually recommended, especially regarding reproductive health.
Corrective Surgery
When significant symptoms, fertility issues, or pregnancy complications occur, surgery may be considered. This procedure aims to unify the two uterine horns to create a more functional cavity. Due to its complexity, it is performed only in select cases.
Assisted Reproduction Treatments
For women facing difficulty achieving pregnancy, reproductive medicine can greatly improve success rates. In vitro fertilization (IVF) is often recommended.
Complications of a Bicornuate Uterus
A bicornuate uterus does not always cause complications, but it is important for women with this condition to receive appropriate medical follow-up to minimize risks.
Infertility
The abnormal shape of the uterus can hinder embryo implantation and increase the risk of infertility.
Recurrent Miscarriage
Women with a bicornuate uterus have a higher likelihood of recurrent pregnancy loss due to:
- Limited space for fetal growth
- Cervical incompetence
- Poor uterine tissue quality or vascularization
- Abnormal embryo positioning
Preterm Birth
Many women with this condition may experience preterm delivery before 37 weeks of gestation.
Abnormal Placenta Position
This condition may increase the risk of placenta previa or abnormal implantation, leading to bleeding or restricted fetal growth.
Tips for Women With a Bicornuate Uterus
If you’ve been diagnosed with this malformation, don’t panic. Each case is unique, and many women with a bicornuate uterus have healthy, successful pregnancies. Regular follow-ups with a specialist are essential.
Always Consult a Specialist
A gynecologist can assess your individual case and provide recommendations tailored to your needs.
Family Planning
A bicornuate uterus does not necessarily prevent pregnancy, but it is important to discuss reproductive plans with your doctor. They may recommend ovulation monitoring, controlled ovarian stimulation, or in vitro fertilization.
Specialized Pregnancy Care
Because complications may occur, pregnancy should be monitored as high-risk. Warning signs include vaginal bleeding, intense pain, or early contractions.
Emotional Support
Accepting this condition can be emotionally challenging. Counseling or joining support groups may help you cope and connect with others facing similar experiences.